- - Deep Brain Stimulation Surgery Pictures
- - What is Deep Brain Stimulation Surgery?
- - How Deep Brain Stimulation Works?
- - Before and After Deep Brain Stimulation Surgery
Viewing images that showcase the entire Deep Brain Stimulation (DBS) surgery, from electrode placement to pulse generator implantation and final programming, offers a clear visual understanding of how this advanced system works and its role in managing neurological symptoms.
At Turkey Luxury Clinics, we use detailed pictures to explain the DBS device, its effects, the surgical steps, and what patients can expect, helping answer key questions and make the process easier to understand.
Deep Brain Stimulation Surgery Pictures
Deep Brain Stimulation (DBS) surgery involves the precise placement of electrodes in targeted brain regions and connection to a small pulse generator implanted under the chest skin. Viewing images of DBS surgery, from stereotactic frame setup, lead implantation, to pulse generator insertion, provides a clear visual understanding of the procedure. These pictures illustrate how each component works together to deliver controlled electrical stimulation, helping manage movement and neurological disorders effectively.
What is Deep Brain Stimulation Surgery?
Deep Brain Stimulation (DBS) is a neurosurgical procedure used to treat movement and neurological disorders by implanting electrodes in targeted areas of the brain and connecting them to a small pulse generator under the skin.
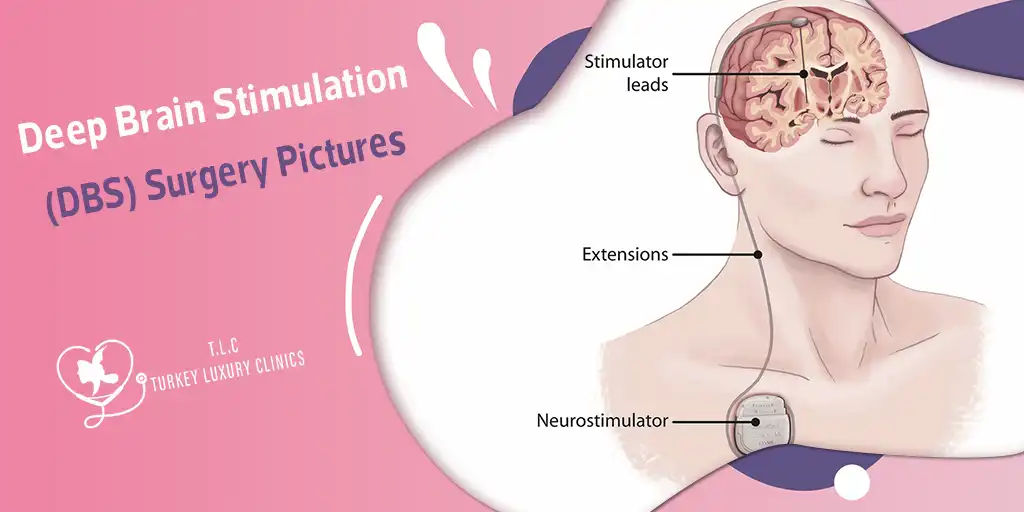
Illustration of Deep Brain Stimulation (DBS): electrodes implanted deep in the brain are connected via insulated leads to a neurostimulator (pulse generator) placed under the skin — allowing targeted electrical stimulation to regulate abnormal neural activity.
This illustration highlights how electrical pulses travel through the DBS system: the neurostimulator in the chest generates signals that pass through the extension wires and reach the implanted brain electrodes. These signals help stabilize abnormal activity responsible for symptoms such as tremors, rigidity, and slowness, allowing patients to regain smoother and more predictable movement without destroying any brain tissue.
Medical illustration showing the internal components of a Deep Brain Stimulation (DBS) system. A thin electrode is implanted in a specific target area of the brain, connected through extension wires to a neurostimulator placed under the skin in the chest. The device delivers continuous, programmable electrical stimulation, and can be externally adjusted by clinicians to match the patient’s changing needs and optimize symptom control.
Schematic diagram of DBS surgery showing electrode placement, connection through extension wires, and implantation of the pulse generator in the chest for controlled stimulation.
Coronal schematic of the brain showing the implanted stimulating electrode targeting the ventral capsule/ventral striatum (VC/VS), highlighting the deep-brain placement of the lead used in DBS therapy
How Deep Brain Stimulation Works?
DBS surgery is usually performed in two major steps. First, the electrodes are implanted in the targeted brain region and connected to an extension wire beneath the scalp. In the second stage, a pulse generator similar to a pacemaker is placed in the chest and attached to the extension wire. After surgery, the doctor programs the pulse generator to deliver customized electrical stimulation that best controls the patient’s symptoms.
1. Determination site of Lead placement
The image shows an anatomical diagram of the basal ganglia and thalamus with three deep brain stimulation (DBS) leads placed in their typical treatment targets. One lead is positioned in the VIM, which is commonly used for tremor control, another in the STN, and a third in the GPi — both of which are key targets for treating Parkinson’s disease and other movement disorders.
Before your DBS surgery, the neurosurgeon needs to determine where the electrodes will be placed depending on the treated condition and affected brain area. usually by using pre surgical MRI. Electrode locations and numbers vary by type of disease and symptoms. This step is crucial for optimal results.
2. DBS Frame, Drill, and Incision Making
The image shows the patient’s head secured in a DBS stereotactic frame. Surgical instruments are positioned for a precise skull opening (small craniotomy), enabling careful electrode insertion while minimizing risk and ensuring accuracy.
To ensure precise electrode placement, your head is fixed using a stereotactic frame. The surgeon then makes a very thin opening using a drill, allowing safe insertion of electrodes into the targeted brain areas.
3. Lead Implantation (Awake vs Asleep)
Intraoperative view of a patient undergoing DBS surgery — showing surgical positioning and equipment during lead implantation.
This intraoperative photo shows a patient awake during DBS surgery, raising their hand while the neurosurgeon touches a finger to test responsiveness. This step allows the surgical team to confirm accurate electrode placement in the brain, ensuring optimal stimulation and symptom relief. Awake testing is a crucial part of the procedure for safety and effectiveness.
Illustration of ClearPoint MRI-guided DBS with skull-mounted stereotactic frame and trajectory device for precise electrode placement under real-time imaging.
This image shows the use of imaging during DBS surgery. Intraoperative MRI (A) helps the surgeon plan the exact placement of electrodes in the thalamus to treat essential tremor. Fluoroscopy (B) confirms accurate positioning of the electrodes during surgery, and postoperative CT scans (C) verify their final placement, ensuring safe and effective stimulation.
Recent studies show asleep-DBS can provide similar or better outcomes than awake-DBS for speech, cognitive function, and patient comfort. Modern MRI/iMRI/CT guidance allows precise electrode placement without relying on patient feedback. Awake-DBS is still performed in specialized centers for real-time testing of neurological function.
4. Pulse‑Generator Implantation
DBS pulse generator implanted under the chest skin, connected via extension wires to brain electrodes, delivering controlled electrical stimulation.
X-ray view of a Deep Brain Stimulation (DBS) system showing the pulse generator implanted in the chest. The extension wire travels up the neck and connects to the intracranial electrodes, providing a detailed technical perspective of the full hardware configuration within the patient.
During the Deep Brain Stimulation (DBS) procedure, the pulse generator—a small, battery-powered device—is implanted under the skin, usually in the upper chest area. This device connects to the electrodes placed in the brain via a thin extension wire, enabling controlled electrical stimulation to manage neurological symptoms.
5. Programming and Activation
This image shows the programming setup for a DBS system. Clinicians use the patient programmer to adjust stimulation parameters, fine-tuning the device for symptom relief and patient comfort.
After the pulse generator is implanted, the DBS system is programmed and activated. A neurologist or trained clinician uses a patient programmer or specialized device to adjust the stimulation settings. This process ensures the electrical impulses are tailored to the patient’s symptoms, optimizing symptom control while minimizing side effects.
Before and After Deep Brain Stimulation Surgery
The image highlights how targeted electrical stimulation helps reduce tremors and improve motor control, demonstrating the therapeutic impact of the implanted DBS system.
DBS can significantly improve symptoms such as tremors, rigidity, and slow movements. Before surgery, patients may experience noticeable hand tremors, stiffness, and difficulty with everyday tasks. After DBS activation, images often show smoother, more controlled movements, with a marked reduction in tremors and improved motor coordination. Patients frequently report easier hand control and a reduction in involuntary movements, which can greatly enhance daily functioning and quality of life.









.webp)
.webp)
.webp)
.webp)

