- - How Many Times Can You Have a Corneal Transplant?
- - Keys for Successful Repeat Corneal Transplant
- - What is a Secondary or Repeated Corneal Transplant Surgery
- - Signs You Might Need a Repeat Cornea Transplant
- - Reasons for Repeating a Corneal Transplant
- - Factors Affecting Success and Longevity of Corneal Grafts
- - Life Span of Repeated Corneal Transplants
- - FAQs About How Many Times Can You Have Corneal Transplant
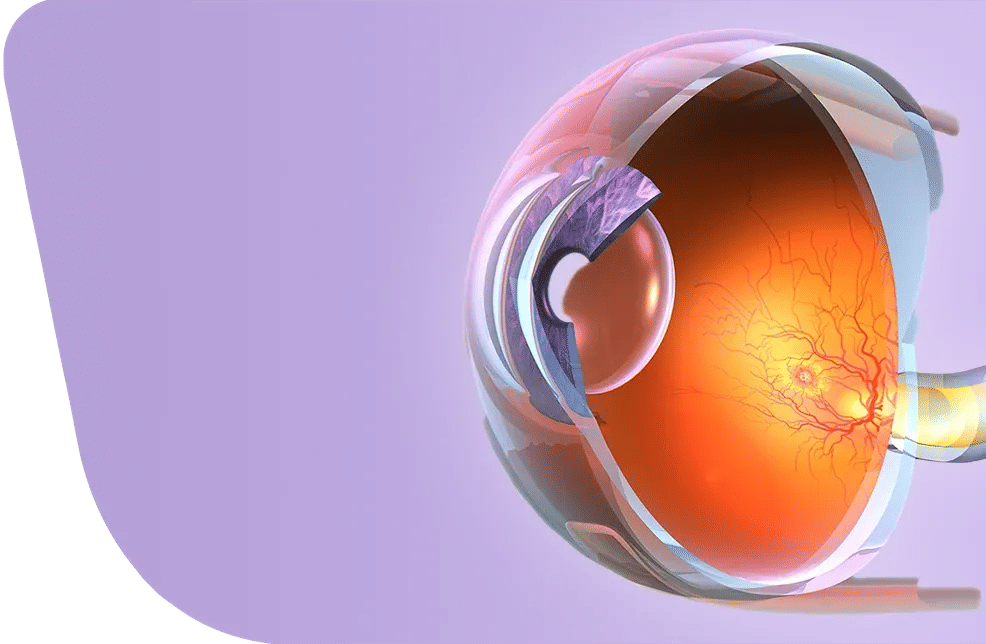
A successful corneal transplant usually lasts 10 to 15 years, and some grafts may survive 20 years or more. However, certain eye conditions can cause the graft to fail earlier.
Failed corneal grafts can be replaced by a secondary corneal transplant, though these subsequent grafts may not last as long as the first one, and some patients may require additional transplants over time.
So, how many times can you have a corneal transplant? Corneal transplants can be repeated multiple times more than once, depending on individual circumstances. Before considering a repeat procedure, factors such as eye health, suitability for surgery, costs, and donor cornea availability should be carefully evaluated.
How Many Times Can You Have a Corneal Transplant?
Corneal transplants can be performed multiple times if needed, as there is no fixed limit and no maximum number of times. Repeat transplants are usually considered when the first graft fails due to rejection, infection, disease recurrence, scarring, or poor vision.
Each subsequent transplant carries a higher risk of rejection and may have a shorter survival period. However, as long as the eye and patient can tolerate the procedure and there is a reasonable chance of success, additional transplants can help restore vision.
Keys for Successful Repeat Corneal Transplant
- Identify the reason for the first graft failure: Understanding why the previous transplant failed helps prevent repeating the same problem.
- Evaluate eye condition: If other eye issues can affect the success of the surgery.
- Choose the type of transplant: Donor cornea is better but artificial cornea is safer
- Understand risks and recovery: Be prepared for complications and necessary follow-up care.
- Prepare your home: Make sure your environment supports healing and reduces strain on your eyes.
- Check availability and cost: Ensure a compatible donor is available and consider the financial aspect.
- Set realistic expectations: Vision may improve, but results are not guaranteed.
- Risk of rejection: The chance of immune rejection is higher than with the first graft.
What is a Secondary or Repeated Corneal Transplant Surgery
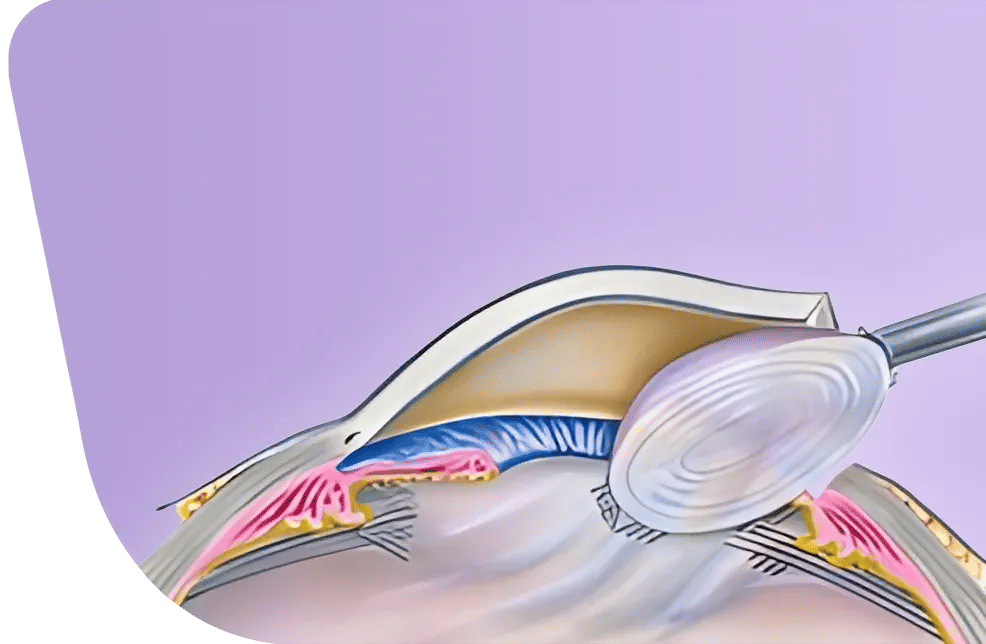
A secondary or repeated corneal transplant is a surgery that replaces a previously transplanted cornea with a new one. This surgery is performed when the previous graft has failed, become cloudy, or caused poor vision to restore sight, improve the clarity of the cornea, and sometimes reduce pain
A corneal transplant can be performed using either a donor cornea (natural cornea) or an artificial cornea.
While the donor cornea is less available and carries a risk of immune rejection, it is usually preferred over the artificial cornea, which is usually a last-resort option, used when a donor cornea is not available or the risk of rejection is high.
Although repeat transplants carry a higher risk of immune rejection than the first graft, they still provide a meaningful chance to regain vision.
Signs You Might Need a Repeat Cornea Transplant
Look out for the classic RSVP symptoms: Redness, Sensitivity to light, Vision changes, and Pain, which often indicate graft rejection. Other warning signs include persistent swelling (edema), infections, or serious complications like glaucoma or retinal detachment. Contact your ophthalmologist if you feel:
- Cloudy or Hazy Vision: Your vision becomes blurry or dim despite previous transplant.
- Scarring or Opacity: Corneal scarring or cloudiness interferes with light entering the eye.
- Pain or Discomfort: Persistent eye pain or irritation that wasn’t present before.
- Decreased Visual Function: Trouble reading, driving, or performing daily tasks.
- Recurrent Swelling or Inflammation: Ongoing corneal swelling that doesn’t respond to treatment.
Reasons for Repeating a Corneal Transplant
You may need a repeat corneal transplant if the first one fails due to immune rejection, natural graft failure from aging or wear, scarring, irregular shape (astigmatism), or if underlying eye conditions like glaucoma limit vision despite a clear graft. Common reasons include:
- Immune rejection: The transplanted cornea is foreign tissue, so your body may reject it, either soon after surgery or later. If patients do not follow the medication prescribed by the surgeon to suppress the immune response, the risk of rejection is high. However, even with correct medication use, some patients’ immune systems may still reject the cornea.
Risk of corneal graft rejection mainly applies to natural donor corneas. Artificial corneas generally have a lower risk of immune rejection. Immune rejection is the most common reason for repeat corneal transplant.
- Infection or inflammation: Eye infections or severe inflammation after surgery can damage the graft. These conditions trigger immune activity that can harm the new cornea and cause scarring, which may make a repeat transplant necessary.
- Disease recurrence: Some underlying conditions that caused the first transplant to fail may also affect the new graft over time. For example:
- Fuchs’ dystrophy: Can cause corneal swelling and cloudiness due to endothelial cell loss.
- Keratoconus: May continue to distort the cornea, even after a transplant
- These issues may eventually lead to graft failure, increasing the likelihood of needing another transplant.
- Scarring or cloudiness: The cornea can become cloudy or scarred due to injury, surgical complications, or natural degeneration. Cloudiness prevents light from entering the eye clearly, reducing vision and potentially necessitating a repeat transplant.
- Poor visual outcome: Even if the corneal graft survives and remains clear, some patients may not achieve good vision. If the cornea is clear but vision remains poor due to scarring, irregular shape, or other eye conditions, the result is considered a suboptimal outcome. In such cases, a repeat corneal transplant may be needed to try to improve sight.
Factors Affecting Success and Longevity of Corneal Grafts
- Type of corneal transplant: Partial-thickness corneal transplants (Deep Anterior Lamellar Keratoplasty, DALK) usually last longer and fail less often than full-thickness corneal transplants (Penetrating Keratoplasty, PK)
- Eye health: Pre-existing eye conditions, infections, or inflammation can make the transplant fail sooner, increasing the chance you’ll need a repeat surgery.
- Immune response: If your body has rejected a previous graft, the risk of rejection in the next transplant is higher.
- Patient age: Younger patients are more likely to need multiple transplants over their lifetime because their eyes are more reactive and they live longer.
- Advanced techniques: Newer procedures, like endothelial keratoplasty (EK), can help the graft last longer and reduce the need for another transplant.
- Underlying condition: Certain conditions, like keratoconus, often allow the transplant to last many years, lowering the chance of needing another surgery.
- Post-surgery care: Following your doctor’s instructions and using medications like steroid eye drops as prescribed improves the success and lifespan of the transplant.
Life Span of Repeated Corneal Transplants
A first corneal transplant can last 10–20 years or more, but repeat grafts usually have a shorter survival time. Each subsequent transplant carries a lower chance of long-term success than the previous one.
To improve the success and longevity of a repeat transplant:
- Select the appropriate type of cornea: Patients at high risk of rejection may benefit from an artificial cornea rather than a donor cornea.
- Use advanced techniques when available, such as 3D-printed custom corneal tissue, which can provide high-precision and personalized grafts.
- Avoid corneal rejection: Follow medications and the doctor’s instructions carefully, especially immune-suppressing medications to reduce the risk of rejection.
- Attend regular follow-ups with your ophthalmologist to catch any complications early.
You may also like
Diabetic Retinopathy surgery in Turkey












.webp)
.webp)
.webp)
.webp)

